Seizures
The brain controls how the body moves by sending out small electrical signals through the nerves to the muscles. Seizures, or convulsions, occur when abnormal signals from the brain change the way the body functions.
Seizures are different from person to person. Some people have only slight shaking of a hand and do not lose consciousness. Other people may become unconscious and have violent shaking of the entire body.
Shaking of the body, either mild or violent, does not always occur with seizures. Some people who have seizures have symptoms before the seizure (auras) or briefly lose touch with their surroundings and appear to stare into space. Although the person is awake, he or she does not respond normally. Afterwards, the person does not remember the episode.
Not all body shaking is caused by seizures. Many medical conditions can cause a type of body shaking that usually affects the hands and head (tremors).
A small number of people will have only one seizure during their lifetime. A single seizure usually lasts less than 3 minutes and is not followed by a second seizure. Any normally healthy person can have a single seizure under certain conditions. For instance, a sharp blow to the head may cause a seizure. Having one seizure does not always mean that a serious health problem exists. But if you have a first-time seizure, you should be checked by your doctor. It is important to rule out a serious illness that may have caused the seizure. Fever seizures (febrile convulsions) are the most common cause of a single seizure, especially in children. For more information, see the topic Fever Seizures.
Causes of seizures
Epilepsy is a nervous system problem that causes seizures. It can develop at any age. For more information, see the topic Epilepsy.
A seizure can be a symptom of another health problem, such as:
- A rapidly increasing fever (fever seizure).
- An extremely low blood sugar level in a person who has diabetes.
- Damage to the brain from a stroke, brain surgery, or a head injury.
- Problems that have been present since birth (congenital problems).
- Withdrawal from alcohol, prescription medicine, or illegal drugs.
- An infection, such as meningitis or encephalitis.
- A brain tumor or structural defect in the brain, such as an aneurysm.
- Parasitic infections, such as tapeworm or toxoplasmosis.
Symptoms:
General
- The person may yell or cry out.
- Stiffen.
- Difficulty breathing (look for pale or bluish skin).
- Jerking motions.
- Falling.
- May last 1-4 minutes.
Treatment:
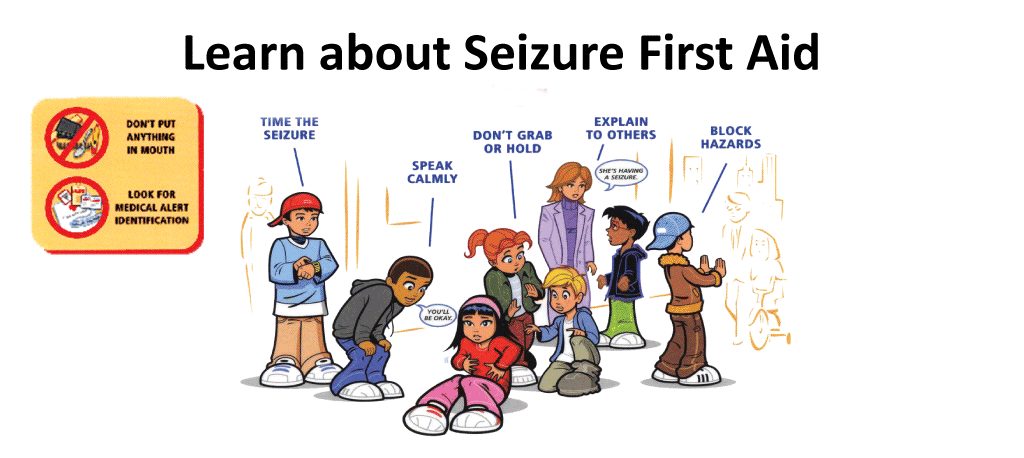
- Remain calm.
- Move all sharp edged objects out of the persons way to help keep them from injuring themselves.
- Monitor their breathing.
- Do NOT try to restrain the person, you cannot stop the seizure.
- Do not force anything into the persons mouth or give them anything to eat or drink.
- Once the seizure has subsided.
- Help the person lay down and place something soft under their head.
- Turn them to one side so they don’t risk choking on their saliva.
- Remove tight or restricting clothing and jewelry.
- The person will probably feel confused and disoriented.
- They will also be very tired, let them sleep but stay with them until they have awoken and are fully awake and alert/aware.
- Do not give them anything to eat or drink until they have fully recovered.
Call emergency if
- If this is a first time.
- If the seizure lasts more than 5 minutes.
- If the person has one seizure after another.
- If the person is pregnant, injured, diabetic, or has requested an ambulance.
- If the person is not breathing correctly within one minute after the seizure. If needed begin CPR.
Prevention:
Note: If you think you may have a seizure disorder or are being evaluated for one, do not drive, operate heavy machinery, swim, climb ladders, or participate in other potentially dangerous activities until you have been specifically cleared to do these things by your doctor.
Many causes of seizures, such as some forms of epilepsy, cannot be prevented. But head injury is a common cause of seizures and epilepsy that you may be able to prevent. To prevent a head injury:
- Wear your seat belt when you are in a motor vehicle. Use child car seats.
- Do not use alcohol or other drugs before or during sports (such as soccer, football, horseback riding, or bicycling) or when operating an automobile or other equipment.
- Wear a helmet and other protective clothing whenever you are bicycling, motorcycling, skating, kayaking, horseback riding, skiing, snowboarding, or rock climbing.
- Wear a hard hat if you work in an industrial or construction area.
- Do not dive into shallow or unfamiliar water.
- Prevent falls at home by removing hazards that might cause a fall.
First aid video for seizures -2