First aid – Wrist Injury
Overview:
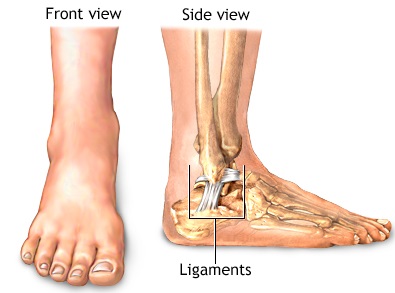
The wrist is made up of the two bones of the forearm (the radius and ulna) and eight carpal bones (scaphoid or navicular, lunate, triquetrum, pisiform, trapezium, trapezoid, capitate, and the hamate). Many ligaments connect these bones to each other.
A sprain is an injury to the wrist ligaments without any evidence of bone injury (that is, no broken bones or cracks in the bone). With a sprain, there is usually only a partial tearing of the ligaments. In a severe wrist sprain, there can be a complete tear.
A fractured or broken wrist means there is a break or a crack in one or more of the bones of the wrist.
A strain is where there is a tearing of the muscle fibers in the area surrounding the wrist.
Definition:
A sprain is an injury to a ligament. Ligaments are strong bands of connective tissue that connect one bone to another.
A wrist sprain is a common injury. There are many ligaments in the wrist that can be stretched or torn, resulting in a sprain. This occurs when the wrist is bent forcefully, such as in a fall onto an outstretched hand.
Alternative Names:
Transverse wrist fracture; Dinner-fork deformity of the wrist.
Types of wrist injury:
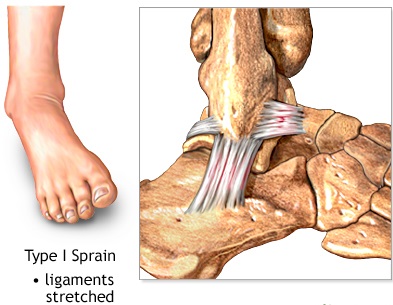
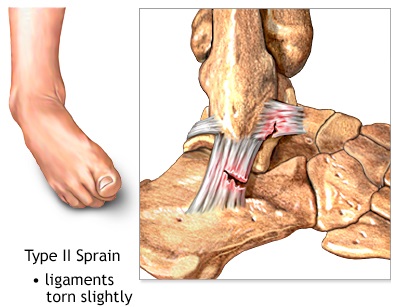
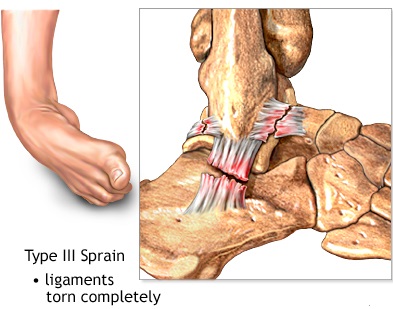
Wrist sprains can range from mild to severe. They are graded, depending on the degree of injury to the ligaments.
- Grade 1: These mild sprains occur when the ligaments are stretched, but not torn.
- Grade 2: These moderate sprains occur when the ligaments are partially torn. Grade 2 sprains may involve some loss of function.
- Grade 3: These severe sprains occur when the ligament is completely torn. These are significant injuries that require medical or surgical care. As the ligament tears away from the bone, it may also take a small chip of bone with it, called an avulsion fracture.
Causes:
This injury usually occurs when a person attempts to break a fall by throwing the hands and arms out in front of them. The hands meet the ground with the body weight behind them. The radius and ulna (the bones in the forearm) may buckle or break just above the wrist.
This injury is more likely to happen during sports such as rollerblading, skateboarding, running, or any other activity in which a forward fall can occur while a person is moving at a higher speed.
Bones become more brittle (from osteoporosis) in adults ages 50 – 60 and older. Older adults are more likely to fracture a bone, even while walking slowly.
The most common cause of wrist injuries is a fall on an outstretched hand:
- You can also have wrist pain from repetitive use that results in an inflammation of the tendons (tendonitis). This is termed a repetitive motion injury and is really not a true sprain.
- Carpal tunnel syndrome is another common wrist injury that may occur from repetitive motion.
- High force or weight through the wris.
Symptoms:
Symptoms of a wrist sprain may vary in intensity and location. The most common symptoms of a wrist sprain include:
- Swelling in the wrist.
- Pain at the time of the injury.
- Persistent pain when you move your wrist.
- Bruising or discoloration of the skin around the wrist.
- Tenderness at the injury site.
- A feeling of popping or tearing inside the wrist.
- A warm or feverish feeling to the skin around the wrist.
Sometimes, a wrist injury may seem mild with very little swelling, but it could be that an important ligament has been torn that will require surgery to avoid problems later.
Similarly, an unrecognized (occult) fracture may be mistakenly considered a mild or moderately sprained wrist. If left untreated, the broken bone may not heal and will require a surgery that could have been avoided with early, appropriate treatment. The most common example of this is an occult fracture of the scaphoid bone.
It is important in all but very mild cases for a doctor to evaluate a wrist injury. Proper diagnosis and treatment of wrist injuries is necessary to avoid long-lasting stiffness and pain.
First Aid:
- Reassure the injured person.
- Place the hand and wrist in a splint in a normal resting position.
- Place a rigid splint on the underside of the wrist, hand, and forearm.
- Place a padded object such as a sock, wadded cloth, or rolled elastic bandage in the palm.
- Wrap the wrist, hand, splint, and padded object. Do not wrap too tightly, and keep the fingertips uncovered.
- Elevate the wrist or place it in a sling.
- Use an ice pack over the wrist to help reduce swelling.
- Bring the person to an urgent care center or emergency medical facility.
- Do NOT attempt to move or straighten the wrist or hand.
RICE Method:
Mild wrist sprains can usually be treated at home with the RICE protocol.
- R Rest the joint for at least 48 hours.
- I Ice the injury to reduce swelling.
Do not apply ice directly to the skin. Use an ice pack or wrap a towel around the ice or a package of frozen vegetables. Apply ice for about 20 minutes at a time.
- C Compress the swelling with an elastic bandage.
- E Elevate the injury above the level of the heart.
A pain reliever, such as aspirin or ibuprofen, may be helpful. If pain and swelling persist for more than 48 hours, however, see a doctor.
When to Seek Medical Care:![]()
If you have severe pain, deformity, numbness, or are unable to move your wrist, you should call your doctor for an immediate appointment, go to an urgent care clinic, or go to a hospital’s emergency department.
If there is no deformity and the pain is manageable with over-the-counter pain medication, you may want to wait 12-24 hours before deciding whether to call the doctor. If symptoms persist after a day, see a doctor.
If you have obvious deformity, numbness, or severe pain, you need medical attention.
- If there is obvious deformity or severe swelling, there may be a broken bone that needs to be moved back into its normal position.
- There also can be a dislocation where the bones are no longer in the correct position, although they are not broken.
Considerations:
Wrist fractures are common among children and the elderly.
- Children’s bones are soft and tend to get buckle (torus) fractures. These are incomplete fractures on one side of the bone.
- Because bones become brittle with age, a complete fracture is more likely in adults and among the elderly. This is called a Colles’ fracture.
Fractures that are not severe may be placed in a splint and sling, or a lightweight, fiberglass cast.
If the bone is no longer straight because of the fracture, it must be reduced (straightened).
- The health care provider may be able to use local anesthesia and reduce the fracture.
- In other cases, surgery may be needed. The break may need to be fixed with a plate and screws, pins, or other metal or plastic hardware.
Older people with Colles’ fractures often fail to regain full mobility of the wrist joint. Carpal tunnel syndrome may occur as an early or late complication of the injury. Chronic pain may result from injury to the ligaments or the joint surface of the wrist.
Prevention:
The following tips may prevent finger, hand, and wrist injuries.
- Do exercises that strengthen your hand and arm muscles.
- Learn safe hand and wrist movements to avoid an injury.
- Reduce the speed and force of repetitive movements in activities such as hammering, typing, knitting, quilting, sweeping, raking, playing racquet sports, or rowing.
- Change positions when you hold objects, such as a book or playing cards, for any length of time.
- Use your whole hand to grasp an object. Gripping with only your thumb and index finger can stress your wrist.
- Consider wearing gloves that support the wrist and have vibration-absorbing padding when working with tools that vibrate.
- Use safety measures, such as gloves, and follow instructions for the proper use of hand and power tools.
- Use caution when using knives in preparing food or craft activities. Supervise a child using knives or sharp scissors in craft activities.
- Wear protective gear, such as wrist guards, in sports activities. Be sure to learn what you can do to help prevent injuries for your child too.
- Review your work posture and body mechanics.
- Organize your work so that you can change your position occasionally while maintaining a comfortable posture.
- Position your work so you do not have to turn excessively to either side.
- Keep your shoulders relaxed when your arms are hanging by your sides.
- When using a keyboard, keep your forearms parallel to the floor or slightly lowered, and keep your fingers lower than your wrists. Allow your arms and hands to move freely. Take frequent breaks to stretch your fingers, hands, wrist, shoulders, and neck. If you use a wrist pad during breaks from typing, it’s best to rest your palm or the heel of your hand on the support, rather than your wrist.
Home treatment for a minor hand or wrist injury:
Home treatment may help relieve pain, swelling, and stiffness.
- Remove all rings, bracelets, or any other jewellery that goes around a finger or wrist. It will be harder to remove the jewellery later if swelling increases.
- Use rest, ice, compression, and elevation (RICE) for pain and swelling.
- Do not use your injured hand or wrist for the first 24 hours after an injury, if possible. An elastic bandage can help decrease swelling. The wrap will also remind you to rest the injured hand or wrist. A wrist splint can help support an injured wrist. Talk to your doctor if you think you need to use a splint or bandage for more than 48 to 72 hours.
- Gently massage or rub the area to relieve pain and encourage blood flow. Do not massage the injured area if it causes pain.
- For the first 48 hours after an injury, avoid things that might increase swelling, such as hot showers, hot tubs, hot packs, or alcoholic beverages.
- After 48 to 72 hours, if swelling is gone, apply heat and begin gentle exercise with the aid of moist heat to help restore and maintain flexibility. Some experts recommend alternating between heat and cold treatments.
- Treat blisters.
Keep your bones strong:![]()
- Eat a nutritious diet with enough calcium and vitamin D , which helps your body absorb calcium. Calcium is found in dairy products, such as milk, cheese, and yogurt; dark green, leafy vegetables, such as broccoli; and other foods.
- Exercise and stay active. It is best to do weight-bearing exercise, such as walking, jogging, stair climbing, dancing, or lifting weights, for 2½ hours a week. One way to do this is to be active 30 minutes a day, at least 5 days a week. In addition to weight-bearing exercise, experts recommend that you do resistance exercises at least 2 days a week. Talk to your doctor about an exercise program that is right for you. Begin slowly, especially if you have not been active. For more information, see the topic Fitness.
- Limit how much alcohol you drink.
- Don’t smoke or use other tobacco products. Smoking puts you at a much higher risk of developing osteoporosis. It also interferes with blood supply and healing. For more information, see the topic Quitting Smoking.
Basic first aid- Treament for wrist injury
Taping to stabilise your wrist painful