Q fever and what causes it?
Q fever (Query fever) is an infectious disease that spreads from animals to humans. Q fever is caused by a microbe called “Coxiella burnetii.” This microbe can survive for months and even years in dust or soil.
Animals such as cattle, sheep, and goats can carry the Q fever microbe in tissues involved in birth–the uterus, placenta, and birth fluids. Infected animals also release the microbe in milk and manure. People acquire the infection by inhaling infectious aerosols and contaminated dusts generated by animals or animal products.
Many infections are without symptoms (asymptomatic). Common symptoms resemble a serious case of the flu with high fever, chills and sweating. In some cases, people develop liver and heart disease.
Q fever transmitted:
People usually contract Q fever when they breathe in the Q fever microbe. It is very infectious. As few as ten Q fever microbes can start an infection. People can also get Q fever by drinking infected milk, and through skin contact but most infections are spread through the air. Person to person transmission occurs rarely, if ever.
What are the symptoms of Q fever:
People can have Q fever without knowing it or mistake it for mild flu. Often, it is impossible to tell without laboratory tests.
Sometimes, Q fever strikes as a sudden illness, affecting a large number of people in the same workplace. Common signs and symptoms resemble a serious case of the flu:
- sudden onset of high fever
- fatigue
- muscle pain
- chills and sweating
- headache
- general feeling of sickness and loss of appetite
Some patients develop a slight, dry cough because of a lung inflammation known as pneumonitis. Most symptoms disappear after 7-10 days. However, afflicted people can feel generally ill with loss of appetite for several weeks.
A small percentage of patients develop hepatitis or liver disease and jaundice, a yellowing of the skin and darkening of the urine, caused by a malfunctioning of the liver.
Other rare clinical syndromes including endocarditis, an inflammation of the lining of the heart cavity, have been reported.
There may be regional differences in the way the disease presents itself. It is not clear why but animal studies suggest different strains may be a factor.
Q fever an occupational concern:
Q fever is an occupational concern for workers who have contact with animals, animal products, or animal waste. Those workers with heart valve problems or suppressed immune systems are at higher risk.
Workers can get Q fever from a variety of different animals:
- farm livestock–especially cattle, sheep, and goats.
- laboratory animals–especially sheep.
- household pets–especially cats
Blood-sucking ticks spread the Q fever microbe to wild animals, but seldom to humans. Farm livestock, laboratory animals, and pets however can pick up Q fever directly from other infected animals or from contaminated surroundings.
Q fever is a special concern with pregnant animals, especially around the time they give birth or abort because of the disease. In pregnant animals, the Q fever microbe builds up to enormous numbers in certain tissues and fluids. These include:
- the uterus or womb,
- the placenta, which surrounds the offspring in the womb,
- the mammary glands or udders,
- birth fluids, and
- milk.
Studies show that one gram of placenta from an infected sheep can contain over one billion Q fever microbes.
These microbes become airborne in tiny droplets of mists or aerosols and spread to workers:
- during processing of infected tissues from slaughtered animals,
- at milking or during the processing of milk, or
After giving birth, animals usually eat their placenta and other tissues of afterbirth. When this happens, the Q fever microbes survive digestion. They pass along the animal’s intestine and become discharged with the manure. This allows Q fever to spread widely throughout the environment.
The Q fever microbe easily becomes airborne with dust from infected animal tissues, manure, or soil. As a result, workers can become exposed to Q fever by contacting various infected materials such as
- dust from animals, bedding, or manure,
- animal hides, wool, and furs, and
- clothes from workers who were exposed to infected animals or materials.
Occupations are at increased risk for Q fever:
Q fever spreads easily throughout agricultural regions affecting anyone who works outdoors in contact with infected soil or dust. Airborne particles containing the Q fever microbe may be carried downwind for a considerable distance–one-half mile or more.
Q fever also spreads easily within buildings from room to room. Workers in research facilities can catch Q fever even if they only visit a contaminated room or hallway once or twice.
General medical staff do not normally get Q fever from infected patients.
Some of the occupations at increased risk for Q fever include the following:
- farmers, ranchers, and farm workers in contact with cattle, sheep, and goats,
- stockyard workers, truck drivers, personnel who service the trucks, and visitors to animal auctions,
- meat packers, rendering plant workers, hide and wool handlers,
- laboratory animal researchers and support staff,
- workers who care for pets and livestock–veterinary personnel, pet shop workers and zoo attendants, and
- certain groups of medical and health care personnel who have contact with blood, sputum or tissue from infected patients.
Prevent Q fever in the workplace:
For most effective prevention, the Q fever microbe should be eliminated from animals. Eradications programs, however, are not yet available because Q fever spreads so effectively among animals. So far, research on vaccination programs for animals has not had practical success.
Workers who have even remote contact with animals, animal products, and animal waste should be informed about the disease, its characteristics, and the nature of the risk. Workers who start jobs with increased risk of Q fever should be offered blood tests to determine if they have resistance to Q fever or whether they should consider vaccination. The possibility of Q fever should be investigated in high risk workers who develop an unexplained feverish illness, especially if lung infections develop. Q fever is a reportable disease in most Canadian jurisdictions.
The risk of infection from the workplace can be reduced by:
- personal precautions, and
Vaccination of workers
A vaccine is available to protect workers exposed to the Q fever microbe. The use of this vaccine should be limited to those at high risk of exposure whose blood tests for resistance to Q fever are negative. Before vaccination, workers must also have a skin test to determine if they are allergic to the vaccine.
Personal precautions
Personal precautions can reduce exposure to the Q fever microbe and possibly prevent it from spreading within the workplace:
- Access to workplaces with increased risk of Q fever should be restricted to workers required to be there.
- Protective clothing should be worn by workers exposed to animal tissue. Contaminated clothing should be labelled with a biohazard warning and washed using laundry procedures for disinfection.
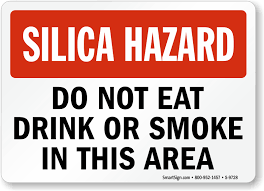
- No eating, drinking, smoking, or nail biting should be allowed in animal holding facilities. Hands should be washed frequently.
- Animal tissue should be handled with care, especially tissue involved in birth.
- Production and exposure to aerosols from animal tissues should be minimized.
- Respiratory protection devices suitable for preventing aerosol inhalation should be used by workers at increased risk of inhaling contaminated droplets.
- Acceptable laboratory techniques as outlined in “Laboratory Biosafety Guidelines” should be used in research or diagnostic laboratories that process blood and tissue from animals or patients with Q fever. “Laboratory Biosafety Guidelines” and other biosafety references are listed elsewhere on this web site.
Workplace hygiene:
Procedures should be developed to prevent the release and spread of the Q fever microbe within the workplace. Each workplace should have procedures to disinfect or sterilize areas that may be contaminated with the Q fever microbe.
- In medical research laboratories associated with hospitals, animals should be kept in separate facilities to reduce the possibility of the Q Fever microbe spreading to staff and patients. Use of common elevators and loading docks should be avoided.
- Pregnant ewes should not be used in research laboratories unless they have negative antibody tests for Q Fever.
- Biosafety containment equipment and facilities should be used in laboratories as recommended in “Laboratory Biosafety Guidelines”.
- When livestock give birth, they should be confined and closely observed. The placenta and other birth tissues should be collected before the animals eat them and disposed of safely.
- Infectious waste should be packaged in puncture-proof, leakproof containers that are clearly labelled and sterilized before disposal according to procedures developed for biological hazards.
- Surfaces, floors, and walls contaminated with fluids or dust from animals should be disinfected using procedures established for infection control.